Introduction on OSHA COVID-19 Guidance on Preparing Workplaces
Coronavirus Disease 2019 (COVID-19) is a respiratory disease caused by the SARS-CoV-2 virus. It has spread from China to many other countries around the world, including the United States. Depending on the severity of COVID-19’s international impacts, outbreak conditions—including those rising to the level of a pandemic—can affect all aspects of daily life, including travel, trade, tourism, food supplies, and financial markets.
To reduce the impact of COVID-19 outbreak conditions on businesses, workers, customers, and the public, it is important for all employers to plan now for COVID-19. For employers who have already planned for influenza pandemics, planning for COVID-19 may involve updating plans to address the specific exposure risks, sources of exposure, routes of transmission, and other unique characteristics of SARS-CoV-2 (i.e., compared to pandemic influenza viruses).
Employers who have not prepared for pandemic events should prepare themselves and their workers as far in advance as possible of potentially worsening outbreak conditions. Lack of continuity planning can result in a cascade of failures as employers attempt to address challenges of COVID-19 with insufficient resources and workers who might not be adequately trained for jobs they may have to perform under pandemic conditions.
What does this focus on ?
The Occupational Safety and Health Administration (OSHA) developed this COVID-19 planning guidance based on traditional infection prevention and industrial hygiene practices. It focuses on the need for employers to implement engineering, administrative, and work practice controls and personal protective equipment (PPE), as well as considerations for doing so.
This OSHA COVID-19 Guidance is intended for planning purposes. Employers and workers should use this planning guidance to help identify risk levels in workplace settings and to determine any appropriate control measures to implement. Additional guidance may be needed as COVID-19 outbreak conditions change, including as new information about the virus, its transmission, and impacts, becomes available.
OSHA WEB PAGE :
The OSHA COVID-19 webpage offers information specifically for workers and employers: www.osha.gov/covid-19.
About COVID-19
Symptoms of COVID-19
Infection with SARS-CoV-2, the virus that causes COVID-19, can cause illness ranging from mild to severe and, in some cases, can be fatal. Symptoms typically include fever, cough, and shortness of breath. Some people infected with the virus have reported experiencing other non-respiratory symptoms. Other people, referred to as asymptomatic cases, have experienced no symptoms at all.
According to the CDC, symptoms of COVID-19 may appear in as few as 2 days or as long as 14 days after exposure.
How COVID-19 Spreads
The virus is thought to spread mainly from person-to-person, including:
- Between people who are in close contact with one another (within about 6 feet).
- Through respiratory droplets produced when an infected person coughs or sneezes. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
It may be possible that a person can get COVID-19 by touching a surface or object that has SARS-CoV-2 on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the primary way the virus spreads.
People are thought to be most contagious when they are most symptomatic (i.e., experiencing fever, cough, and/or shortness of breath). Some spread might be possible before people show symptoms; there have been reports of this type of asymptomatic transmission with this new coronavirus, but this is also not thought to be the main way the virus spreads.
Although the United States has implemented public health measures to limit the spread of the virus, it is likely that some person-to-person transmission will continue to occur.
How a COVID-19 Outbreak Could Affect Workplaces
Workers could be absent because they are sick; are caregivers for sick family members; are caregivers for children if schools or day care centers are closed; have at-risk people at home, such as immunocompromised family members; or are afraid to come to work because of fear of possible exposure.
2. Change in patterns of commerce.
Consumer demand for items related to infection prevention (e.g., respirators) is likely to increase significantly, while consumer interest in other goods may decline. Consumers may also change shopping patterns because of a COVID-19 outbreak. Consumers may try to shop at off-peak hours to reduce contact with other people, show increased interest in home delivery services, or prefer other options, such as drive-through service, to reduce person-to-person contact.
3. Interrupted supply/delivery.
Shipments of items from geographic areas severely affected by COVID-19 may be delayed or cancelled with or without notification.
Steps All Employers Can Take to Reduce Workers’ Risk of Exposure to SARS-CoV-2
- Develop an Infectious Disease Preparedness and Response Plan
- Prepare to Implement Basic Infection Prevention Measures
- Develop Policies and Procedures for Prompt Identification and Isolation of Sick People, if Appropriate
- Develop, Implement, and Communicate about Workplace Flexibilities and Protections
- Implement Workplace Controls
Engineering Controls
Engineering controls involve isolating employees from work-related hazards. In workplaces where they are appropriate, these types of controls reduce exposure to hazards without relying on worker behavior and can be the most cost-effective solution to implement. Engineering controls for SARS-CoV-2 include:
- Installing high-efficiency air filters.
- Increasing ventilation rates in the work environment.
- Installing physical barriers, such as clear plastic sneeze guards
- Installing a drive-through window for customer service.
- Specialized negative pressure ventilation in some settings, such as for aerosol generating procedures (e.g., airborne infection isolation rooms in healthcare settings and specialized autopsy suites in mortuary settings).
Administrative Controls
Administrative controls require action by the worker or employer. Typically, administrative controls are changes in work policy or procedures to reduce or minimize exposure to a hazard. Examples of administrative controls for SARS-CoV-2 include:
- Encouraging sick workers to stay at home.
- Minimizing contact among workers, clients, and customers by replacing face-to-face meetings with virtual communications and implementing telework if feasible.
- Establishing alternating days or extra shifts that reduce the total number of employees in a facility at a given time, allowing them to maintain distance from one another while maintaining a full onsite work week.
- Discontinuing nonessential travel to locations with ongoing COVID-19 outbreaks
- Developing emergency communications plans, including a forum for answering workers’ concerns and internet-based communications, if feasible.
- Providing workers with up-to-date education and training on COVID-19 risk factors and protective behaviors (e.g., cough etiquette and care of PPE).
- Training workers who need to use protecting clothing and equipment how to put it on, use/wear it, and take it off correctly, including in the context of their current and potential duties. Training material should be easy to understand and available in the appropriate language and literacy level for all workers
Safe Work Practices
Safe work practices are types of administrative controls that include procedures for safe and proper work used to reduce the duration, frequency, or intensity of exposure to a hazard. Examples of safe work practices for SARS-CoV-2 include:
- Providing resources and a work environment that promotes personal hygiene. For example, provide tissues, no-touch trash cans, hand soap, alcohol-based hand rubs containing at least 60 percent alcohol, disinfectants, and disposable towels for workers to clean their work surfaces.
- Requiring regular hand washing or using of alcohol-based hand rubs. Workers should always wash hands when they are visibly soiled and after removing any PPE.
- Post handwashing signs in restrooms.
Personal Protective Equipment (PPE)
While engineering and administrative controls are considered more effective in minimizing exposure to SARS-CoV-2, PPE may also be needed to prevent certain exposures. While correctly using PPE can help prevent some exposures, it should not take the place of other prevention strategies.
Examples of PPE include: gloves, goggles, face shields, face masks, and respiratory protection, when appropriate. During an outbreak of infectious diseases, such as COVID-19, recommendations for PPE specific to occupations or job tasks may change depending on geographic location, updated risk assessments for workers, and information on PPE effectiveness in preventing the spread of COVID-19. Employers should check the OSHA and CDC websites regularly for updates about recommended PPE.
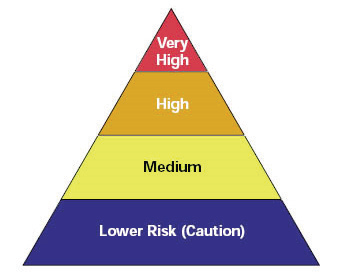
Occupational Risk Pyramid for COVID-19
CHECK ALSO 👇